Living with Parkinson’s disease can feel like an uncharted path. After all, as you will undoubtedly hear countless times along your journey, this is a very personalized disease that affects everyone differently, and symptoms can vary in intensity from person to person.
That being said, there are quite a few commonalities and general things that you can expect. Most importantly, Parkinson’s is a progressive neurological condition that affects movement and brings with it a mix of symptoms that tend to worsen over time.
This progression has been divided into distinct stages, and understanding these stages is essential for patients and families because each stage has its own set of challenges and opportunities for care. By recognizing these stages, you can better prepare for what lies ahead and find ways to manage the journey together with your medical team.
That’s the point of this page: to break down what you can expect in each of those stages so that you know what you’re up against.
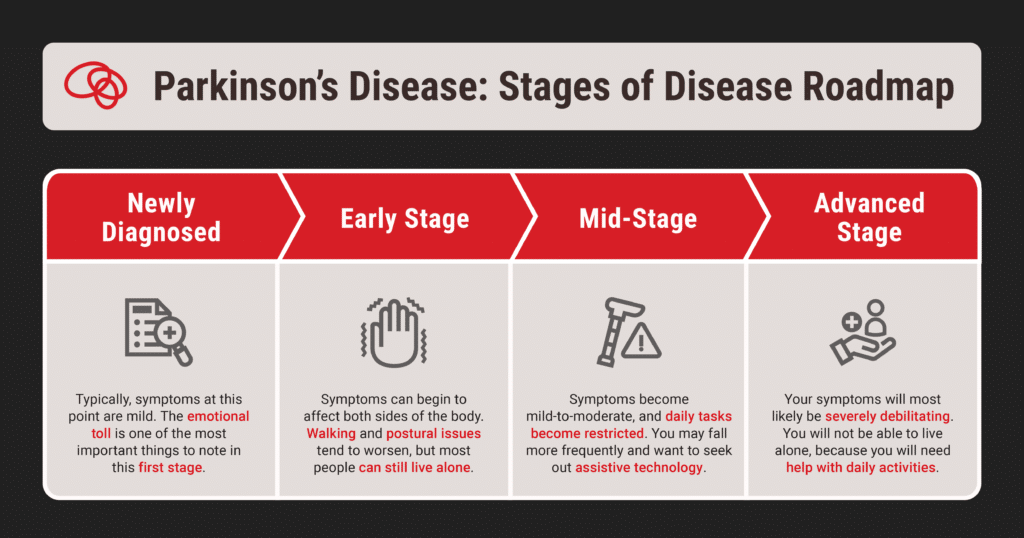
A Roadmap of Parkinson’s Stages
For the purpose of this page, we’re going to assume that you (or your loved one) has recently been diagnosed. Even if the doctor says that you are in a more advanced stage, we think you’ll find some value in the “Newly Diagnosed” section, because many of the things you will experience are similar regardless of how advanced the disease is.
As you read this, keep in mind that the severity of Parkinson’s isn’t something that’s really measurable, and this isn’t meant to be an end-all be-all description of what your journey will look like. We’re just trying to give you a sense of what a typical Parkinson’s trajectory looks like.
Newly Diagnosed
Feeling overwhelmed? Scared? Sad? Uncertain? Numb? Receiving a diagnosis of Parkinson’s is often accompanied by a mix of emotions. You might even feel a strange mix of relief at finally knowing what’s wrong… accompanied by a sense of doom since Parkinson’s currently has no cure. It’s… a lot.
Typically, the symptoms you experience in this first stage won’t strongly interfere with your daily activity. You might have to deal with mild symptoms like tremors, changes in posture, or a slight reduction in facial expressions.
You’ll notice we used the word “mild” in that last paragraph to describe the symptoms in this initial stage. Keep in mind that everything is relative. “Mild” only means that the symptoms will gradually worsen as the disease progresses.
Many people say that these physical changes make them feel frustrated and disheartened. In fact, the emotional toll is one of the most important things to note in this first stage, because you can’t help but grapple with the anxiety of what lies ahead and how the diagnosis may affect your daily life and relationships.
To navigate this challenging time, it’s essential to take proactive steps:
- Educate yourself about the disease
- Connect with support groups
- Establish an open line of communication with healthcare providers
- Engage in mindful activities to process feelings and adjustments
Remember, you’re not alone, and seeking support is a crucial part of the start of this journey.
What Current Patients Say About the Importance of Having Support and Grieving Diagnosis
“I highly recommend connecting with a PD support group…Having conversations and seeing others is an important dynamic even with social media groups… You’ll go through emotional stages with this diagnosis. The 1st year or two is the toughest that way. Together we’re stronger so reach out.”
“There are plenty of moments of grieving the changes, but letting myself feel that pain so I can get to the acceptance on the other side without getting caught in self-pity has opened the door to lots of moments of joy or learning or connection.”
Early Stage
This stage is very similar to the diagnosis stage. Symptoms may begin to worsen over time, and daily tasks may be more difficult and take longer to complete, but you are still able to live alone.
However, tremors, rigidity, and other motor symptoms can begin to affect both sides of the body. There may also be progression in walking and postural issues.
Whether you are a patient or a caregiver, this is the stage where it’s recommended that you start looking into home adjustments. Do the research. Learn how you can prepare your living space for the future. Then implement the changes you can. Trust us, you’ll be thankful later.
Such adjustments can include switching to lightweight furniture, adding non-slip mats, installing handrails, and more. Read our home adjustment recommendations here.
Mid-Stage
This stage is where symptoms develop to become mild-to-moderate, and daily tasks can become restricted. Additionally, you may notice that you are falling more frequently as your balance becomes increasingly impaired.
Assistive technology is important to think about at this stage. There are many new resources and technologies available to help you throughout this stage and the coming stages of Parkinson’s, but you have to seek it out. Using assistive technology can help you to worry less and stay more active, which is probably the best thing you can do for yourself.
Some forms of assistive technology include wheeled walkers, scooters, and car transfer aids – all of which make walking and transportation easier as the disease progresses.
Advanced Stage
At this stage of Parkinson’s, your symptoms will most likely be fully developed and severely debilitating. You will not be able to live alone, because you’re going to need help with your daily activities.
Early on in the Advanced Stage you will probably still be able to walk and stand without help. However, you will likely need a cane for safety in case you lose your balance or fall. As the Advanced Stage progresses, stiffness in your legs may make it impossible to stand or walk.
Whether you’re a patient or a caregiver, it’s wise to learn about advanced Parkinson’s now so you can be prepared and deal with any difficult decisions that need to be made. Specifically, planning ahead provides you with the opportunity to think about what you want to happen if you become unwell.
As Parkinson’s progresses, you may find that you have to take a more complicated combination of medications to treat your symptoms. In this stage, you and your healthcare team may decide that the better option is to stop taking medication.
You may also decide to opt for palliative care during this stage. This form of care is a holistic approach to your physical, emotional, mental, and spiritual needs with the goal of making people with worsened symptoms more comfortable. It is important to note that palliative care is not hospice. Palliative care can be done for anyone in an advanced stage of Parkinson’s and does not prevent you from engaging in other treatment.
As you can probably see, this stage of Parkinson’s is incredibly difficult. Because of that, it is vital to have an open conversation with your healthcare team and caregiver about what you want treatment to look like – ideally before you are experiencing advanced Parkinson’s.
Coping During Each Stage
What do Parkinson’s patients say?
“Daily Rules: In order to stay pertinent or helpful, I do something for:
- Myself 2. My wife 3. Someone else 4. Our house/home/yard”
“Weekly Rules: In order to stay engaged and hopeful, I try to:
- Call and talk to someone I’ve not called in a while.
- Visit with someone or a group outside my home.
- Try to meet someone new!”
“Remember, I am living with Parkinson’s! I am not trying to outlive Parkinson’s or get rid of Parkinson’s.”
Maintaining a healthy lifestyle is very likely the most important part of slowing down the progression of Parkinson’s and helping you maintain your quality of life for as long as possible.
Key areas to focus on are diet, exercise, and hobbies. A balanced diet can provide you with plenty of energy – helping you feel your best both physically and mentally. Regular exercise, whether it’s walking, swimming, or even gentle yoga, not only improves strength and flexibility, but also boosts mood and reduces stress associated with this disease.
You should also take advantage of the various types of recommended therapies – and to start doing so as soon as possible. Just a few of the recommended therapies include occupational, exercise, and speech. These therapies can help you in dealing with changes to your symptoms as well as increase your emotional and mental health.
How the Stages of Parkinson’s Impact Caregivers
Caring for a family member with Parkinson’s disease can be both rewarding and challenging. Loved ones often find themselves navigating a complex emotional landscape filled with deep ups and downs.
It can take a huge toll on a caregiver of witnessing someone they care about progressively lose mobility. In order to continue providing the physical and emotional support required of you, it is essential that you take care of yourself as well.
Enlist the help of others so that you can get time off. Seek out support groups for caregivers. Maintain your own social connections and hobbies.
This is a long road not only for your loved one with Parkinson’s, but for you as well. The only way you’re going to get through the journey is to admit that you’re only human and have empathy and understanding for yourself as well.
Need More Help Understanding Your Stage?
Remember, this disease hits everyone in a different way. The best resource for you is your medical team, your caregiver, and you. Not quite sure what stage you’re in? Keep a journal of your daily experiences and any changes that you notice. These observations will be key in helping to determine how your Parkinson’s is progressing and the best way to treat your specific symptoms.